It is not always a toothache that brings us to the dentist. Quite often it is not the teeth that cause problems, but unpleasant sensations in the mouth, red spots on the tongue, burning sensation. These signs are characteristic of a variety of diseases, often systemic, but can serve as symptoms of glossitis – inflammation of the tongue.
Types of glossitis
All inflammatory processes are divided into chronic and acute, independent and secondary, accompanying other diseases. In any case, problems with the tongue signal the presence of a disease, so it is better to immediately consult a doctor. Sometimes glossitis runs without pronounced manifestations, but the doctor during a preventive examination will certainly notice changes in the tongue.
To independent diseases (when only the tongue is affected) include several types of inflammation.
Acute catarrhal glossitis
Most often develops as a result of mechanical damage by sharp edges of destroyed teeth, unfortunate dentures, lollipops and nutshells. It is a sign of allergies, acute respiratory infections or diseases of the gastrointestinal tract.
Patients have red spots on the root of the tongue . When eating and talking, patients experience pain. The tongue swells, covered with a dense plaque. Saliva secretion increases.
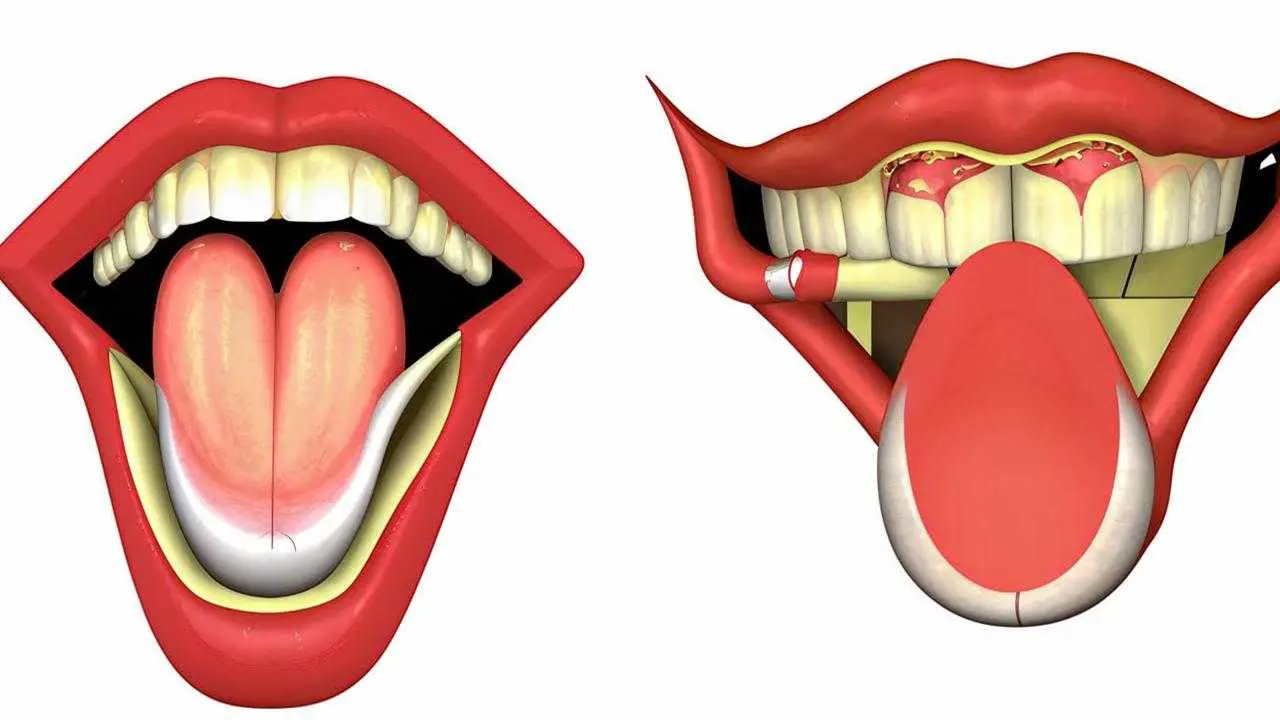
Desquamative glossitis
He has many names: geographic tongue, migrating, exfoliative glossitis. It is he who begins with spots on the tongue of red color. This occurs due to the detachment of the epithelium (desquamation).
The causes are not completely clear, but a certain role in the development of inflammation is played by diseases:
- stomach and intestines;
- endocrine glands;
- hematopoietic organs.
Provoke inflammation can infectious diseases and avitaminosis.
All of them disrupt the nutrition of tissues and as a result, the epithelium begins to slough. Red spots proliferate. As the spots increase, the process of keratinization begins in the center, and the keratinized areas, on the contrary, begin to peel off. So glossitis “migrates” from one part of the tongue to another. In this case, its outline resembles a map, hence the name “geographical”.
In the vast majority of desquamative glossitis is detected during preventive examinations. For a long time he does not cause discomfort. But in neglected cases, the tongue begins to react to spices, sour. There are complaints of tingling, burning. The tongue is covered with cracks, in which infection can penetrate. In this case, the disease is accompanied by an increase in lymph nodes, general malaise, weakness.
Rhomboid glossitis
This is an inflammation of the tongue in which red spots have clear boundaries and geometric shape.
Among the causes are distinguished:
- congenital nature of the disease;
- diseases of the gastrointestinal tract;
- candidiasis of different nature and location.
There are 3 types of rhomboid inflammation. Flat kind – the easiest, patients do not suspect about it, and only the doctor can see the characteristic red spots on the root of the tongue.
Bumpy and papillomatous types are irritated by the sensation of a foreign body in the mouth. Sometimes patients complain of burning.
Black “hairy” tongue
With desquamative glossitis, the epithelium is too peeled off. When the keratinized epithelial cells stop peeling off altogether, we speak of a “hairy tongue”. The size of the papillae increases. They change color as a result of the interaction of iron in food and oral microflora. Most often the papillae become black or brown.
The cause may be:
- gastritis;
- colitis;
- infections;
- tuberculosis;
- venereal disease;
- smoking;
- alcoholic beverages in excessive amounts.
The disease develops gradually and for a long time patients do not pay attention to the changes. Therefore, the sight of a “hairy” tongue can cause great stress. Patients complain of burning, itching, dryness, sensation of a foreign body. Sometimes, gagging occurs when talking. Taste sensations are often altered.
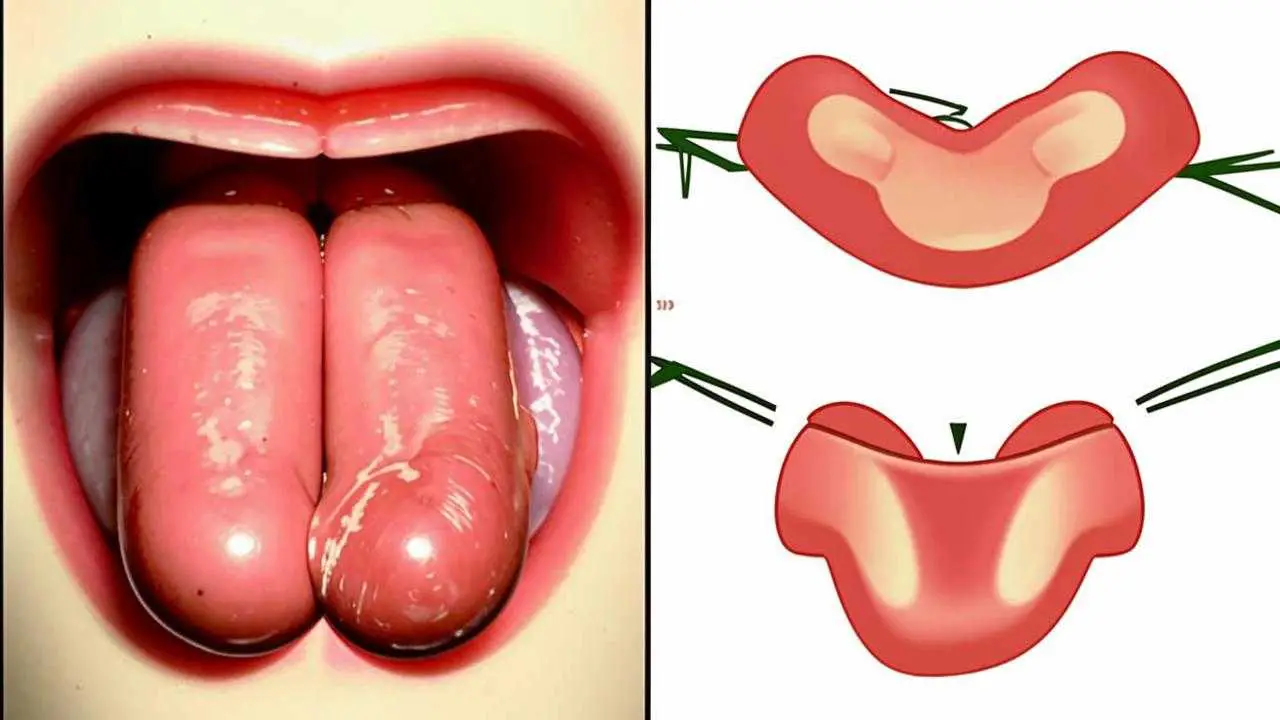
Folded tongue.
This congenital anomaly is detected in children and adults. In children, it is diagnosed less often due to the fact that the folds are small. During the period of intense growth, in puberty, with the growth of muscle tissue increases and the tongue, the folds are manifested more clearly. It is characterized by a change in the shape and size of the tongue. Transverse folds are more shallow, longitudinal – well pronounced. The main problem of pathology is the accumulation of food residues, bacterial products in the folds. For microorganisms, this is a favorable environment. They penetrate into small cracks and provoke the development of other forms of glossitis. In particular, in 50% of cases, the folded tongue is combined with migratory glossitis. Often inflammation is provoked by fungal infections, for example, candidiasis.
There is no specific treatment. In the presence of fungal infection, drugs with fungicidal action, ointments against fungus are prescribed. It is recommended to carefully observe oral hygiene and together with brushing teeth, clean the tongue with special scrapers.
Glossodynia
Glossodynia is a burning syndrome in the mouth. It usually begins with the appearance of red spots on the tip of the tongue. The tongue feels sardonic and tingling. Pain appears, which subsides during meals, but increases in the evening. In 80% of patients, saliva secretion decreases. The tongue swells, desquamation (epithelial detachment) begins. The tongue becomes covered with cracks.
The most common causes
Sometimes, the causes of glossitis are congenital, for example, with a folded tongue. But most often the disease develops on the background:
- Chemical and thermal burns. Putting garlic gruel on a sore tooth may not be such a good idea. And hot food is harmful to the mucosa of the tongue and stomach.
- Infections. Has a red spot appeared on your tongue and it hurts? This can be a symptom of fungal (candidiasis), viral (herpes), bacterial (Helicobacter, spirochete, staphylococcus, streptococcus) infection.
- Mechanical injuries. Gnawing nuts is dangerous not only for the teeth, but also for the mucous membrane of the mouth and tongue. Sometimes constant mechanical impact is caused by incorrect dentures.
- Deficiency of vitamins, especiallyof the B group. This affects tissue metabolism, as a result, the mucosal surface becomes inflamed.
- Psychoneurological factors. With stress, neurological disorders, the tongue becomes inflamed quite often.
Treatment of glossitis of the tongue
First of all, the treatment plan depends on the type of inflammation. It is made individually, based on clinical and diagnostic data. For acute catarrhal glossitis, it is important to remove the irritating factor: replace the crowns or, conversely, put crowns on the destroyed tooth. Change food habits, refuse to chew nuts, hard candies, breadcrumbs.
For a folded tongue, oral hygiene comes to the forefront.
If, with rhomboid glossitis, tubercles and papillomas grow, they are excised. Laser surgery allows you to do this quickly, practically without blood.
The main recommendation for black tongue – treatment of somatic diseases and smoking cessation. Apply liquid nitrogen to reject the papillae, as well as applications to the keratinized areas.
But there is a general approach to treatment:
- Oral sanitation;
- professional teeth cleaning;
- vitamin complexes;
- iron preparations for anemia;
- for pain – light anesthetics in the form of applications;
- for burning – oral baths and irrigation;
- physiotherapy treatments;
- testing for fungal infections.
On the Internet there are many recommendations for the treatment of glossitis with folk remedies. No one disputes the anti-inflammatory properties of chamomile, sage and plantain. When a spot popped out on the tongue, relief can bring applications of sea buckthorn oil and aloe juice. But these measures are temporary, they affect the symptoms, and the cause of the disease remains without attention. As a result, it is easy to miss the moment when it was not difficult to eliminate the problem.
Glossitis is closely related to general diseases and psychological causes. Effective treatment is possible only when using a comprehensive approach. What to treat glossitis and what examinations to undergo can advise only a qualified doctor. Cure glossitis fairly quickly, but if you run, can form abscesses, tumors, necrotic changes in tissues. This is already much more serious and the prognosis is not so favorable.
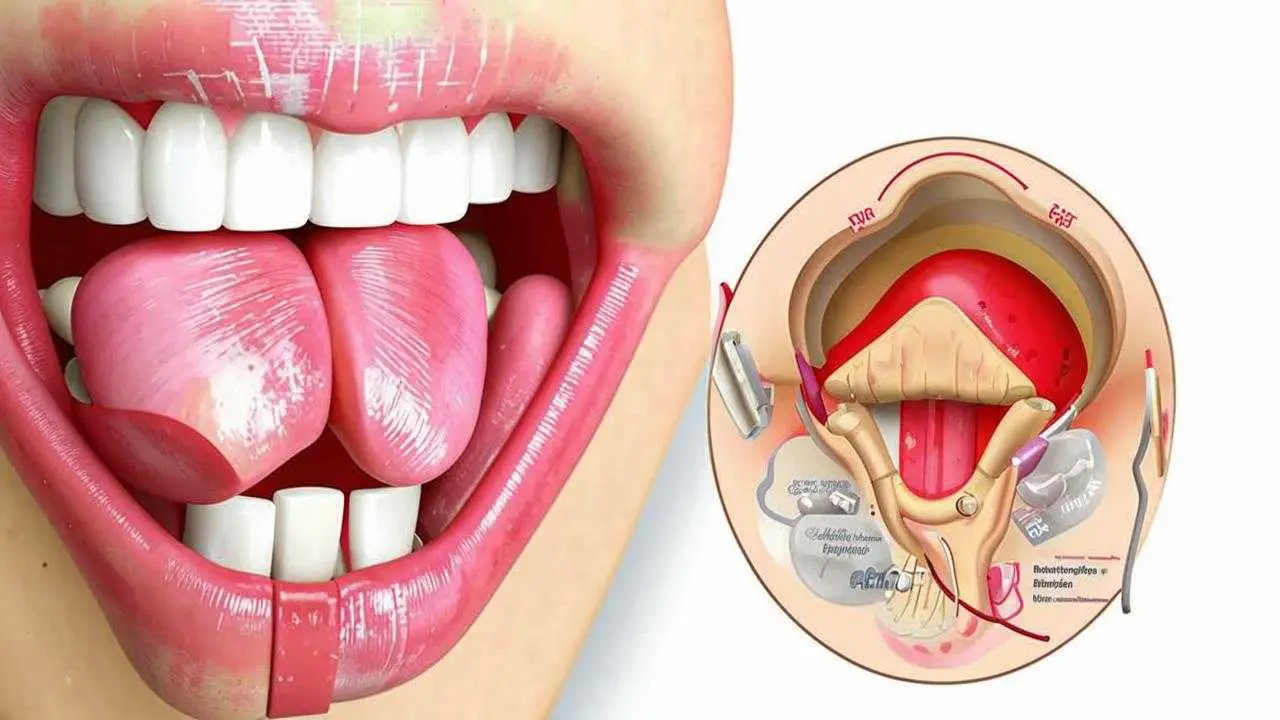
Diagnosis
Visual inspection already gives the dentist an idea of what kind of inflammation is presented in each specific case. But glossitis is important to distinguish from other diseases that manifest themselves in the form of reddish spots: red flat fever, glossalgia, syphilis and tuberculosis. For this purpose, specific examinations are prescribed, which help to understand why red spots appeared on the tongue.
Prevention
Dentists do not get tired of repeating that ordinary hygiene procedures help to prevent a lot of problems. The same recommendations apply to inflammatory diseases of the oral cavity:
- regular brushing;
- flossing;
- refusal to chew nuts, seeds, breadcrumbs;
- irrigation of the oral cavity.
Tips from the ROOTT Clinic dentist on tongue hygiene:
A healthy lifestyle, proper nutrition, smoking cessation have a positive effect on the overall condition of the body, significantly reducing the risk of inflammation.