Periodontal disease is a dystrophic lesion of the tissues surrounding the tooth and holding it in the alveolus (dental cavity). It is accompanied by atrophy of certain areas of the periodontium, sclerotic changes in bone tissues, reduction of bone mass, gingival recession, exposure of tooth necks and increased sensitivity. As the disease progresses, the height of the alveolar process decreases, the gingival joints are completely destroyed, the bone walls of the tooth cells resorb, leading to tooth loss.
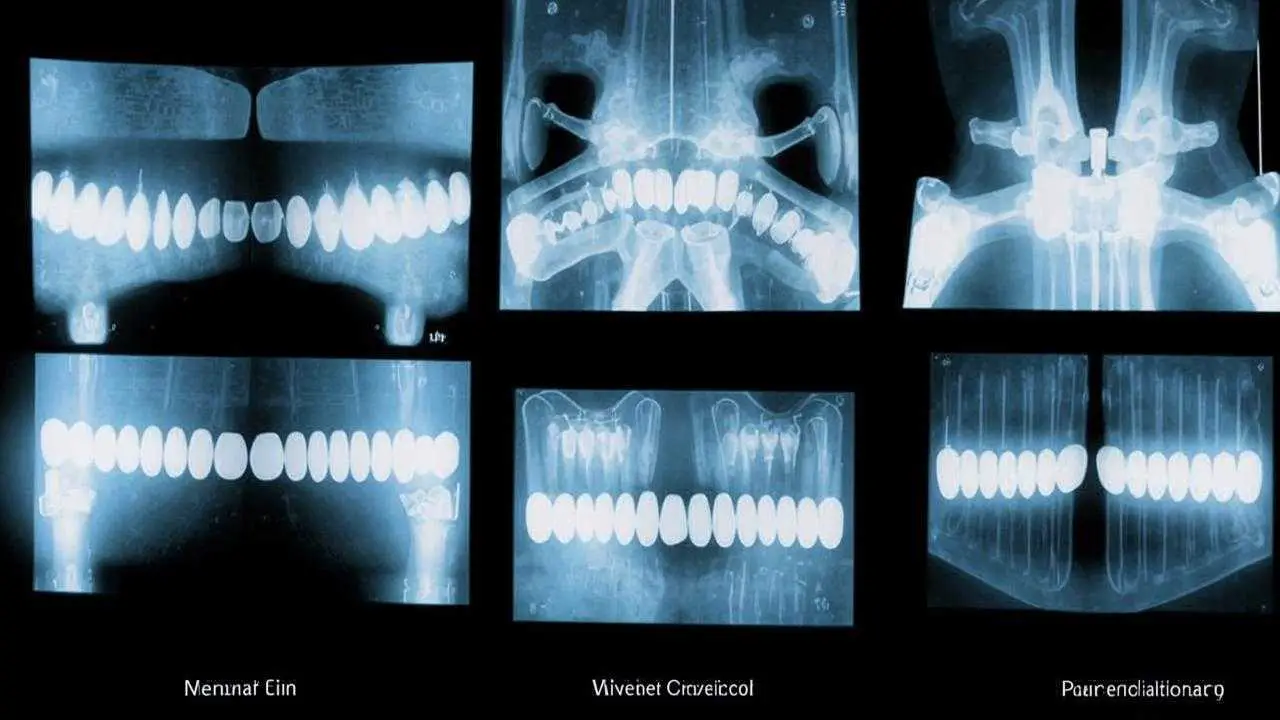
The disease is characterized by a slow course, clinical signs are manifested with significant destructive changes in the periodontium. Diagnosis is made on the basis of clinical picture, the results of X-ray examination. Only a dentist can notice the beginning of pathological changes in periodontal tissues. If the patient sees the symptoms of periodontal disease, then the disease has been going on for many years.
Symptoms
Detect the symptoms of periodontal disease at the initial stage can only be detected by X-ray examination. On the radiograph, sclerotic changes in the bone, changes in its pattern, a decrease in the height of the interalveolar septa are noted. Although there are no pronounced manifestations in the initial stages of the disease, the following changes should alert:
- Minor itching, discomfort in the gums;
- there is sensitivity of teeth to temperature, chemical irritants;
- gums have become pale, dense;
- the enamel has changed color;
- increased interdental spaces;
- gingiva decreased in height.
The first signs of periodontal disease, forcing to seek help from a dentist, are manifested by significant morphological changes in the tissues – this is an increase in the length of crowns, exposure of dental roots, which is especially noticeable in the anterior section of the dental arch. The condition of gum pockets does not change. With a significant decrease in the height of the alveolar ridge (12 root lengths or more), there is pathologic mobility of the teeth.
The severity of symptoms depends on how deeply the atrophy has affected the peri-dental tissues. Depending on the spread of the destructive process, periodontal disease is divided into generalized (the entire tooth row is affected) or localized (the roots of the teeth in a certain area of the jaw are exposed).
Classification
According to the severity of destructive changes, there are light, medium and severe degrees of periodontal disease.
Stage I (initial)
The mild form is characterized by slight itching, burning in the gums, a slight subsidence of the gum with denudation of the tooth necks, increased sensitivity of the teeth for cold, hot, sour. On the background of infectious-inflammatory diseases (acute respiratory viral infections, influenza, etc.) redness, swelling of the gingiva is possible. On the radiograph, the initial signs of bone atrophy are noted.
Stage II (middle)
The middle stage is accompanied by denudation of the neck and root of the tooth up to 2-3 mm, bone loss, slight mobility of teeth in the wells, increase in interdental spaces. Movable teeth traumatize gingival tissue, it periodically becomes inflamed, there is bad breath, purulent discharge from under the gum. The image shows bone destruction of more than 13 times the length of the tooth root.
Stage III (severe)
At the severe stage, the height of the alveolar process is significantly reduced, pathological mobility of the teeth is expressed. They are barely held in the wells, often displaced, rotated on the axis. Some teeth have completely resorbed bone bed, they fall out without pain, blood. The gingiva is pale colored, periodontal pockets are not present, dental deposits are insignificant or absent. Or vice versa – the gingiva is inflamed, blood and pus are released from it. On the radiograph – pronounced horizontal resorption of the jawbone with foci of osteosclerosis, osteoporosis.
Causes of periodontal disease
- Atherosclerotic changes in blood vessels;
- pathologies of the gastrointestinal tract;
- hypovitaminosis;
- endocrine disorders;
- metabolic disorders in oral tissues;
- heredity;
- bite defects;
- neglect of oral hygiene;
- periodontal traumas;
- bad habits (heavy smoking, alcoholism);
- osteopenia;
- decreased immunity.
Possible complications
Atrophy of tissues, destruction of the peri-dental ligament deprive the unit of natural support. Teeth loosen, shift, fall out, which seriously affects not only the beauty of the smile. The normal function of chewing is disturbed, leading to problems with the gastrointestinal system. Periodontal disease can be complicated by periodontitis, inflammation of regional lymph nodes (lymphadenitis), osteomyelitis of the jaws, periostitis, phlegmon of the peri-mandibular spaces and neck (in the presence of alveolar abscesses).
Diagnosis
The doctor establishes the diagnosis based on the results of examination and laboratory-instrumental studies. Examination includes:
- collection of anamnesis, identification of complaints;
- dental examination – checking the sensitivity of teeth, assessing the state of the gums, enamel, the degree of exposure of the necks of teeth, probing gum pockets;
- orthopantomogram, CT scan;
- general, biochemical blood analysis.
If indicated, additional tests may be prescribed (immunogram, Rotter’s test to detect vitamin C deficiency, etc.).
Differential diagnosis of periodontal disease in ROOTT dentistry is carried out with eosinophilic granuloma, periodontitis, tooth mobility on the background of trauma. Accompanying inflammation of periodontal tissues may cause some difficulties in making an accurate diagnosis.
The main differential-diagnostic signs of periodontal disease:
- Absence of pathologic gingival pockets;
- Preservation of the cortical plate in the presence of sclerotic changes;
- fine-cellular bone pattern;
- uniform reduction of interalveolar septa;
- horizontal type of resorption with foci of osteoporosis, osteosclerosis.
Based on the results of diagnosis, a treatment plan is drawn up. The main set of measures is aimed at restoring and normalizing tissue blood flow, eliminating the cause of the disease, stimulation of regeneration processes in the periodontium.
How to treat periodontal disease
Treatment is complex, carried out by a periodontist together with a therapist, endocrinologist (if indicated). The main goal is to preserve the patient’s teeth, improve the functionality of the dentoalveolar apparatus. Treatment is long, labor-intensive, requires the patient to precisely follow the doctor’s recommendations and appointments. The therapeutic plan is made taking into account the degree of damage to periodontal tissues.
Methods of treatment of periodontal gum disease include drug therapy, physiotherapy, surgery, local and general impact on the pathological process in the periodontium:
- professional hygiene (removal of supragingival, subgingival deposits);
- caries treatment, filling of root defects;
- instrumental treatment of bone pockets, altered root surfaces;
- layer-by-layer infiltration;
- creation of bone tissue mineral depot (physiotherapy with calcium preparations);
- restoration of the correct bite;
- elimination of deformities caused by decreased occlusal height;
- orthopedic treatment.
A separate cure for periodontal disease has not yet been found. The disease is treated comprehensively. The process involves sanitation of the mouth, correction of hygiene, the use of special pastes, rinses. It is important to correct nutrition, sleep, saturate the diet with vitamins, minerals, carefully care for the oral cavity, regularly massage the mucosa. In the initial stages of the disease, treatment is maximally effective, provides a good, stable result. In periodontitis of medium, severe degree, it is almost impossible to achieve complete remission, but to stabilize the process for several years – the task is quite realistic.
Drug therapy
The main disease is treated, symptomatic therapy is prescribed:
- means to improve blood circulation;
- antibacterial drugs;
- immunomodulators;
- antiseptics (mouthwash);
- vitamin therapy – folic acid, vitamins of group B, A, C, P, E are injected into the gums or by electrophoresis;
- drugs that improve tissue regeneration;
- plasma therapy to improve blood circulation, slowing atrophy.
Vitamins in periodontal disease strengthen bone tissue, contribute to the restoration of dentin, activate periodontal nutrition, normalize carbohydrate, protein metabolism, stimulate mineral metabolism, fight inflammation of the gums, accelerate healing, restore oral microflora, strengthen capillary walls, normalize oxidation reactions. Treatment of periodontal disease becomes more effective, goes much faster.
Vitamin therapy is combined with the intake of mineral complexes. For the health of teeth, bone tissue need calcium, phosphorus. Their assimilation is facilitated by vitamin D. The integrity of bone structures is disturbed in the deficiency of fluorine, zinc, iron. Replenish the reserves of trace elements will help vitamin and mineral complexes (Vitrum, Complivit, Multi-tabs, Elevit). They satisfy the daily need for useful substances, and they do it quickly.
Injections into the gums with periodontal disease
Local exposure to solutions, ointments on the gums, often turns out to be insufficiently effective. The doctor prescribes injections into the gums, in this case, the drug quickly penetrates under the gum, acting with maximum efficiency. Effective remedy for periodontal disease is selected individually, according to the clinical picture, the general state of health. The course of treatment – 2-4 weeks with an interval of 1 day.
Physiotherapy
In the treatment of periodontal disease, the following physiotherapeutic methods are used:
- gum massage;
- electrophoresis;
- darsonvalization;
- gingival shower;
- ultrasound, laser therapy;
- use of magnetoform applicators;
- hydro-gas-vacuum massage;
- acupuncture, acupressure.
Physical procedures are carried out in courses, in combination with local therapy.
Hardware therapy
Hardware treatment of periodontal disease is aimed at restoring metabolism in the gum cells. VECTOR and VARIUS devices, diode laser Opus 5 and Velur S9 are used. The method effectively removes all soft, hard dental deposits, even if they are located deep under the gum. Laser treatment eliminates inflammation, swelling, normalizes blood circulation, metabolic metabolism, accelerates the regeneration of periodontal tissues. Modern devices successfully treat even complex forms of the disease, allowing in many cases without surgical intervention.
Orthopedic treatment
To increase the resistance of teeth, irritating factors are eliminated:
- Align occlusal surfaces;
- selective grinding;
- temporary or permanent splinting;
- prosthetics.
The question of the necessity of installing a prosthetic system to reduce the load, splinting of the tooth row, preserving the aesthetics is decided individually.
Surgical treatment
To correct the edge of the mucosa, gingival plasty is performed. The flap method involves transplanting tissue to the area where there is a loss of mucosa. The operation allows you to close the exposed necks of the teeth, restore aesthetics. Such intervention is effective only at the initial stage of the disease, with minor gingival recession. At the same time, drug therapy is prescribed, aimed at restoring intercellular metabolism, activation of tissue regeneration, prevention of further loss of mucosa.
In advanced stages of the disease resort to methods of directed tissue regeneration. Different cell cultures are used as biomaterials, selectively stimulating regenerative processes in the periodontium. Implantation is carried out to restore the dentition in case of pronounced mobility or loss of teeth.
New protocols allow simultaneous removal of non-viable units, replacing them with roots made of titanium – implants. When choosing one-stage techniques with immediate loading, implants are placed in the area with sufficient bone parameters, which makes it possible to avoid sinus elevator, osteoplasty. Loading with the prosthesis is carried out immediately, up to a maximum of 3 days after surgery. In severe cases of severe bone atrophy in the upper jaw, advanced clinics use pterygoid implants, an innovative method, an alternative to traumatic zygomatic implantation.
Is it possible to cure periodontal disease with home remedies
Home treatment of periodontal disease of the teeth is ineffective. Decoctions, gargling with medicinal herbs are not able to cope with bone dystrophy. The use of hydrogen peroxide, various folk mixtures, chemical compositions is not only useless, but very dangerous. Periodontal disease is a serious disease that requires qualified medical assistance. Medicinal herbs can reduce inflammation of the gum, but not restore the volume of bone tissue or prevent mucosal recession. There is no need to self-medicate. It is better to visit a dentist and treat periodontal disease in the clinic.
Is periodontal disease contagious
This is a systemic lesion of peri-dental tissue of a non-inflammatory nature. The disease is not transmitted by airborne or other means, it is impossible to become infected with it. The cause of its development is often systemic diseases of the body (diabetes mellitus, atherosclerosis, metabolic disorders, etc.), heredity or deficiency of useful substances.
Difference between periodontal disease and periodontitis
Periodontal disease | Periodontitis | |
Pathogenesis | Dystrophic lesion of peri-dental tissues of a non-inflammatory nature | Inflammation of periodontal tissues |
Nature of course | Does not go unnoticed for years | Rapidly develops, recurring, acute stages, pronounced symptomatology |
Causes | Not fully understood. Predominantly – systemic diseases of the body, heredity | Poor hygiene, tartar, jaw misalignment, vitamin deficiency. |
Prevalence of the lesion | A segment of teeth or the entire dentition is affected. | May affect 1, several or all teeth in the row. |
Inflammation and bleeding gums | Usually absent | Main symptoms |
Tooth mobility | Occurs when teeth are exposed more than 12 times the root length. | It is observed in the acute phase of the disease, against the background of loose, swollen, bleeding gums. After treatment disappears |
Prognosis | Continuous supportive treatment. In the medium, severe form, the process is only subject to stabilization. The overall prognosis is unfavorable (loss of teeth) | With proper therapy, elimination of symptomatology, full recovery |
Prevention of periodontal disease
- Quality oral care;
- use of dental floss, irrigator to clean hard-to-reach places;
- mouthwash after meals;
- timely diagnosis and elimination of the causes of the disease;
- correction of diet (more vitamins, less carbohydrates);
- regular massage of the gums;
- systematic visit to the dentist.
Separately it should be said about the means of care. They must be chosen competently. Toothpaste from periodontal disease should contain mineral salts. They improve metabolic processes, tissue blood circulation, which is necessary for inflammatory, dystrophic pathologies of the periodontium. The specialist will diagnose the state of the dentoalveolar system, will tell you what kind of paste is better suited for care.