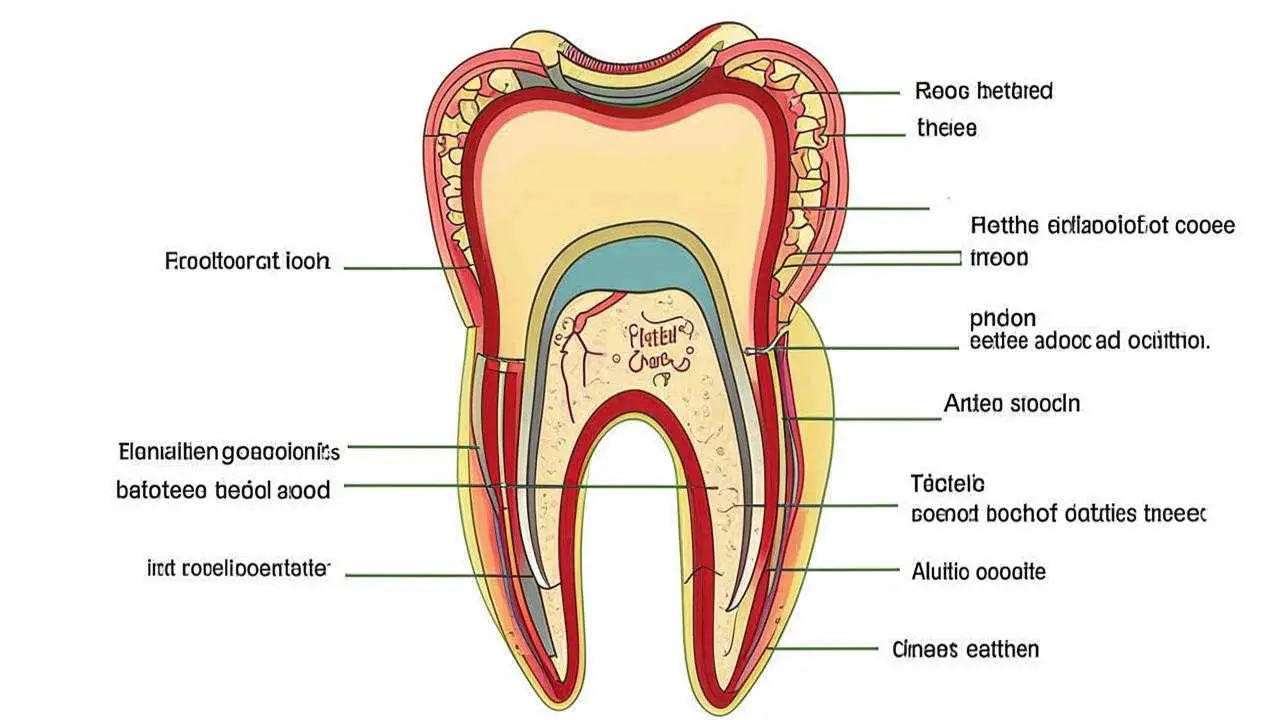
Periodontitis is a periodontal disease of inflammatory nature that leads to destruction of the gingival junction and tooth loss without appropriate treatment. It begins with inflammation of the gingiva, occurring as chronic gingivitis. Later on, the pathological process affects deeper tissues, leading to the destruction of the periodontium, the dental alveolus (cavity), the adjacent jawbone.
The tooth and periodontium is a single functionally and morphologically related system. Damage to its individual elements violates the functionality of the dental unit, leads to a violation of gingival attachment, the formation of deep gingival pockets, the formation of abscesses, fistulas on the gingiva, loosening, loss of teeth.
الأعراض
- Gingival inflammation;
- hyperemia (redness) of the mucosa, swelling, reaction to temperature stimuli;
- gingival soreness;
- discomfort, bleeding gums when chewing, oral hygiene;
- gingival detachment from the tooth wall;
- formation of gum pockets;
- abundant plaque and calculus around the tooth;
- pus from the gums;
- loosening of the gum margin;
- exposure of tooth roots;
- tooth mobility;
- inflammation of the submandibular lymph nodes.
Symptoms of periodontitis vary with the degree of spread of the inflammatory process. The more severe the stage of the disease, the more pronounced the symptomatology. The disease does not occur suddenly, the early stage of periodontitis is catarrhal gingivitis – inflammation of the gingiva, not accompanied by a violation of the integrity of the mucosa.
التصنيف
Periodontitis is classified by localization, the nature of the course, severity.
By the nature of the course
Distinguish acute and chronic form. In the first situation, the signs of periodontitis are pronounced, the gums are loose, bleeding, painful. If the patient does not turn to the doctor or ineffective treatment was prescribed, the disease takes a chronic course. In the chronic form, the symptomatology is smoothed, there are no acute inflammatory phenomena, but the consequences are heavier. For chronic pathology is characterized by periodic exacerbations, when the symptomatology becomes sharply pronounced.
By localization
According to the spread of the pathological process, periodontitis is divided into:
- Localized (focal) – occurs in a small area, in the area of 1 or several teeth.
- Generalized periodontitis – inflammation in the area of all or most of the teeth in the row.
Symptomatology of localized and generalized forms of the disease does not differ, the only difference is the number of teeth around which the pathological process has spread.
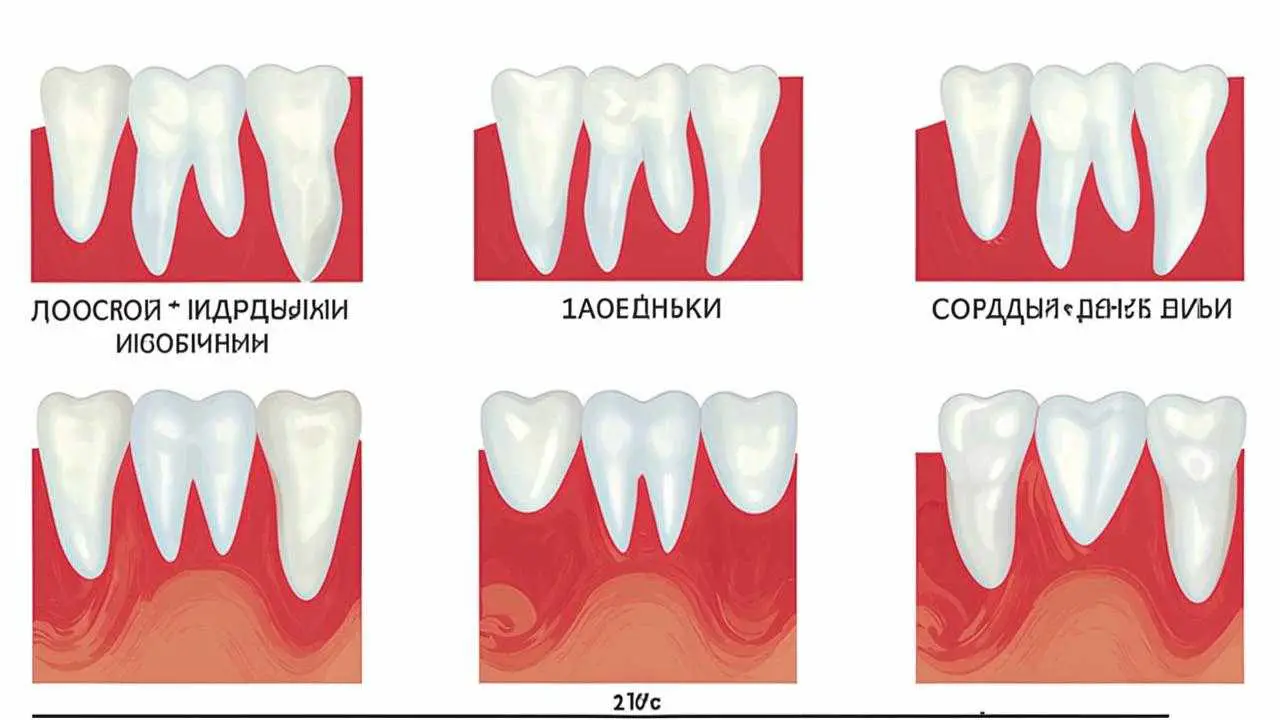
Degrees of periodontitis
- Light – unfolding of the compact plate, reduction of the interalveolar septum up to 13 times the length of the tooth root, signs of osteoporosis, slight tooth mobility, periodontal pockets 2.5-3.5 mm.
- Medium – the depth of periodontal pockets increases to 5 mm, there is moderate mobility of teeth (I-II degree), bone atrophy around teeth reaches 12 roots. There is exposure of tooth necks and roots or inflammatory gingival overgrowth, abscesses (pustules in the gums) may form. Teeth begin to “diverge” under chewing pressure, the gingival margin is deformed. This is especially noticeable in the area of the front incisors. The gums bleed when chewing, brushing, the necks of the teeth are exposed, react painfully to temperature stimuli.
- Severe – symptomatology is increasing, exacerbations of chronic periodontitis in adults are accompanied by the formation of abscesses, sharp swelling of the gum, pain. The depth of periodontal pockets reaches 6 mm, up to the root tip. The interdental spaces increase, there is a strong mobility of teeth (II-III degree), bone resorption, up to complete resorption of the alveolar septum.
Depending on the individual characteristics of the organism, the disease proceeds differently. Aggressive forms of periodontitis are characterized by rapid, almost rapid destruction of periodontal tissues, loosening of teeth, their painless loss. In another part of patients, the disease proceeds slowly, with occasional exacerbations, long remission.
The most severe form is necrotizing periodontitis, in which the gum tissues cease to receive nutrition, blood circulation stops in them, necrosis of the periodontium, periodontal ligaments, alveolar bone occurs. This form of the disease occurs in patients with severe immunodeficiency conditions (AIDS, DiGeorgi syndrome, TKIN, etc.).
Causes of periodontitis
The decisive role in the development of the disease is attributed to the pathogens of dental plaque, which contribute to the inflammation of the gingiva. The accumulating bacterial plaque hardens. Tartar grows, penetrates deep into the gum, because of which the mucosa begins to peel away from the tooth, a free space is formed, which is gradually filled with pathogenic bacteria. Gingivitis develops, which without proper treatment quickly transforms into acute periodontitis.
Factors that provoke the development of periodontitis also include:
- regular traumatization of the gum due to incorrectly installed dentures, orthodontic systems;
- improper occlusion;
- accumulation of food particles, plaque under prosthetic, orthodontic constructions;
- abuse of smoking, alcohol;
- decreased immunity;
- physical trauma to the teeth (impact);
- bruxism.
The development of chronic periodontitis can be affected by problems with the gastrointestinal tract, endocrine disorders, blood diseases, vitamin deficiency, metabolic disorders, insufficient chewing load (predominance of soft food in the diet), autoimmune pathologies, allergies to some drugs.
Possible complications
Periodontitis is a permanent focus of infection in the body. The focus of inflammation grows, involving new, healthy tissues. Disease-causing bacteria penetrating into the general bloodstream, provoke diseases of internal organs and systems, undermine immunity. Due to dystrophic changes in the periodontium, bone tissue, possible deformation of the jaw. In purulent form, fistulas are formed with the exit of pus outside or inside the tissues, which is fraught with the formation of abscesses, phlegmons, the development of sepsis.
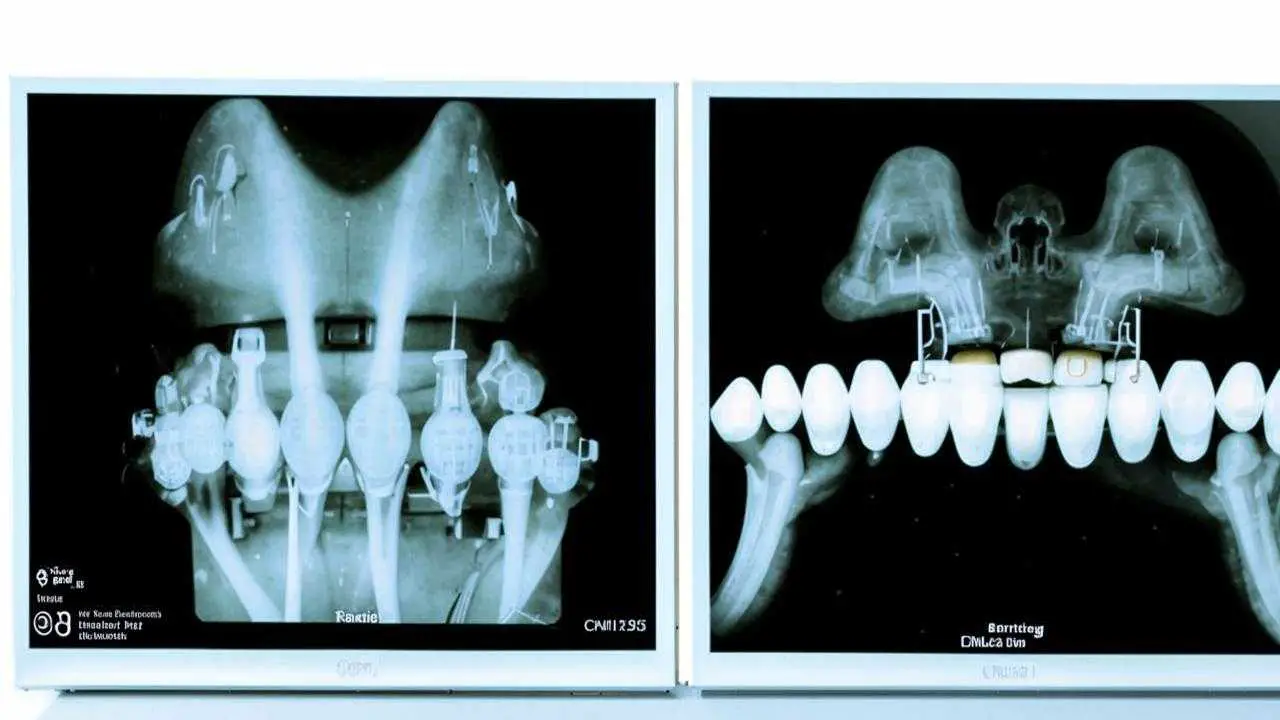
التشخيص
- Collection of anamnesis;
- Dental examination with measurement of the depth of gum pockets (periodontogram);
- Orthopantomogram (OPTG), CT scan;
- reoparodontography (assess the tone of blood vessels);
- Schiller-Pisarev test;
- microbiological studies (PCR);
- blood tests (general, for sugar).
Differential diagnosis of periodontitis is carried out with gingivitis, eosinophilic granuloma of the jaw, periodontal changes in Lefebvre-Papillon syndrome. What methods of examination will be required depends on the form, severity of the disease.
Methods of treatment
Treatment includes a set of local and general measures, prescribed individually, according to the results of examination, according to the severity of the disease, the peculiarities of its course, the general state of health. Effective comprehensive treatment of periodontitis is aimed at eliminating periodontal pockets, strengthening teeth, gums, preventing the destruction of soft and hard tissues.
Hygienic cleaning
Regardless of the stage of the disease, the first stage of treatment is the elimination of all dental deposits. For this purpose, special ultrasonic equipment is used, which allows you to gently remove plaque and calculus even in the most difficult-to-reach places. After curettage (scraping) or ultrasonic cleaning performed with the help of hand tools, the gums are treated with antiseptic, and therapeutic bandages with anti-inflammatory and antimicrobial agents are applied.
Drug therapy
With a mild degree of the disease prescribe local drugs for periodontitis (gels, ointments, solutions for rinsing) with anti-inflammatory, antimicrobial, healing effect. In complex cases, systemic antibiotic therapy is prescribed, taking hormonal, antihistaminic drugs, vitamin and mineral complexes. Conservative treatment is effective at an early stage of the disease.
Preparations for the treatment of periodontitis of the gums have anti-inflammatory, analgesic, antiseptic action. Therapeutic action is provided with the use of medication as solutions for rinsing, applications to the gums, tablets for oral administration, injections into the gums (vitamins, PhyBS, aloe preparations, etc.). The course of treatment – from 2 to 4 weeks with an interval of several days.
Physiotherapy
For the speediest elimination of the infectious focus, active regeneration of tissues, additionally prescribe physiotherapy procedures – ultraphonophoresis, darsonvalization, ozone therapy, electrophoresis, gum massage, laser therapy. Cure localized periodontitis at an early stage can be completely, without resorting to drastic measures. That is why it is so important to contact a dentist at the first alarming signs of the disease.
Orthopedic treatment
In the course of treatment, orthopedic constructions are corrected, parts of fillings are removed from the interdental spaces, crowns that have sagged deeply under the gum or incorrectly installed are re-prosthetized. Splinting in periodontitis is indicated in case of tooth mobility of II degree. Temporary splinting is performed before curettage or immediately after it, permanent splinting – one month after treatment.
Surgical methods
In the severe form of periodontitis, with deep gum pockets, gingival margin defects, in addition to conservative treatment, surgical treatment is required. Radical intervention involves cleaning of gingival pockets with or without gingival dissection, gingivectomy – surgery to remove inflamed, overgrown areas of the gum. The intervention involves reducing the volume of gingival pockets, forming an aesthetic gingival margin. After the procedure, the natural process of tissue regeneration is started. In case of complete resorption of alveolar septa, excessively mobile, non-viable teeth are extracted.
In case of significant destruction of the jawbone, when it cannot firmly hold the tooth in place, osteoplastic surgery – directed bone regeneration – is performed. For this purpose, the area between the tooth and the bone is filled with biocompatible osteoplastic material, which serves as a platform for the formation of new osteoblasts and restoration of bone volume.
Modern periodontitis treatments such as laser and vector therapy are showing impressive results. Already in one procedure gum pockets are reduced, swelling, pain and bleeding disappear. Non-contact methods have a biostimulating effect, significantly accelerate tissue healing. Regardless of the severity of periodontitis, all patients are determined the correctness of occlusion, if indicated, carry out selective grinding of teeth.
Can be treated with home methods
Decoctions of herbs (violet tricolor, calendula, lingonberry leaf, marsh aira, oak bark) will help relieve the symptoms of acute inflammation. But no rinse will not get rid of supra-gingival, and especially sub-gingival dental deposits. Only professional hygienic cleaning in the dentist’s office can cope with this. Folk remedies in the form of hydrogen peroxide, baking soda and lemon will only aggravate the situation. But to maintain the condition of the gums after treatment at home is not only possible, but also necessary. All the necessary recommendations on how to treat periodontitis at home, will give a dentist
Is periodontitis contagious
Periodontitis itself is not contagious. But since pathogenic microorganisms play a major role in its development, they can be transmitted to another person through close contact (kissing).
How to restore teeth at a severe degree of periodontitis
When the disease is severe, the risk of losing a tooth or an entire dentition is very high. Tooth extraction in periodontitis is shown with excessive mobility, when the unit is barely held in the bone, shifts in all directions, around the axis. If it is impossible to save the tooth, orthopedic treatment is performed – prosthetics with the support of own teeth or implants.
In case of single defects or restoration of a segment of teeth, two-stage implantation with delayed loading is used. Implants are implanted after a course of gum treatment, restoration of bone volume. Bone parameters are restored by bone grafting surgery. After the new bone tissue is formed (after 6 months), implants are implanted, the prosthetic system is fixed after their fusion with the jawbone(after 3-6 months). Treatment may take about a year.
Differences between periodontitis and periodontal disease
Periodontal disease
| Periodontitis | |
Pathogenesis | Systemic dystrophic lesion of periodontium | Infectious-inflammatory lesion of periodontium |
Nature of course | Develops slowly, asymptomatic | Rapidly develops, often relapses, symptoms are vividly manifested in the acute period. |
Causes | Predominantly – systemic pathologies of the body, hereditary predisposition | Poor hygiene, abundant bacterial plaque, tartar, improper occlusion, jaw trauma. |
Prevalence | A segment of teeth or the entire dentition is affected | Inflammation is localized in the area of one or more teeth or affects the entire jaw. |
Inflammation and bleeding gums | Absent | Main signs |
Tooth mobility | Occurs with gingival recession of more than 12 times the length of the tooth root. | Observed in the acute period of the disease, against the background of friability, swelling, bleeding gums. After treatment it disappears |
Prognosis | Requires constant, supportive therapy. In the medium, severe form of the process is only subject to stabilization. The overall prognosis is unfavorable (loss of teeth) | With timely treatment, full recovery |
الوقاية
- Thorough oral hygiene twice a day;
- choosing the right toothbrush, toothpaste, rinse;
- use of dental floss, irrigator to clean interdental spaces, hard-to-reach meters;
- balanced diet rich in vitamins;
- strengthening of immunity;
- regular preventive checkups with a dentist(every 6 months), professional cleaning.
Toothpaste for periodontitis belongs to the group of therapeutic and prophylactic. It has a soothing, healing, anti-inflammatory effect. Such pastes often contain extracts, tinctures of medicinal herbs, antiseptics. Therefore, they should be used in courses – no more than 2-3 weeks. The abrasiveness index of toothpaste should be in the range from 20 to 50. Toothbrush should be changed every 3 months.